The Act Phase of PDSA
This phase of the PDSA cycle is where the team implements any changes to the initial plan. Following the Act phase, the PDSA cycle starts over until the outcome has been met. Your team may decide to change some of the process steps to better measure or track performance. Additions to staff education or other methods to promote staff ownership and accountability of the new process could be implemented.
Keeping Track of Progress
In every improvement plan, it is important to track progress, assign responsibility and identify barriers to success. Please see the
Sample Performance Team Agenda and Minutes worksheet your team may find useful. (See Appendix B)
Additional Tools and Resources for Performance Improvement, Teamwork and Staff Engagement
Below are descriptions of tools for use in more complex situations or when you feel you must “dig deeper” into actual or potential problem. Use of these tools in performance improvement can be help to more accurately determine which issues are causing poor compliance in a quality measure.
Another useful source for learning more about performance improvement tools is the Centers for Medicare and Medicaid Services (CMS). Lastly, Stratis Health (stratishealth.org) is a non-profit organization with a mission to support quality and performance improvement. Stratis offers a team of experts and several on-line resources to help you further develop your organization’s plan for quality and ongoing performance improvement.
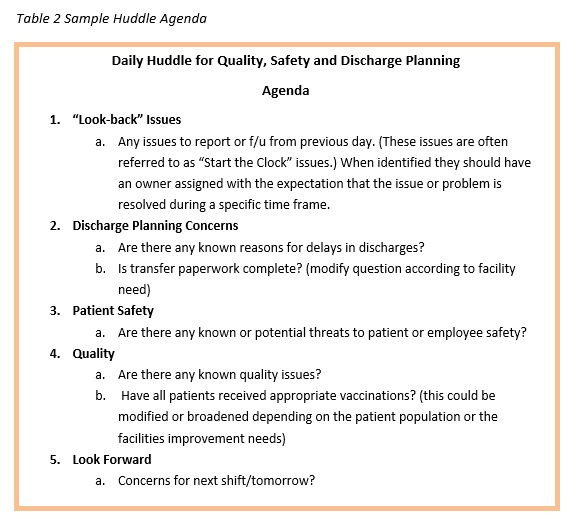
Huddles
Huddles are an excellent way to engage staff in performance measures, provide immediate feedback and instill a sense of comradery for success. Huddles are a structured “stand-up” meeting with a central focus, usually around quality, patient safety and/or discharge planning.
Huddles should be daily, brief (no more than 15 minutes), have a set agenda, and be held with core members of the team who are empowered to solve problems. Typically, huddles are led by the manager or senior leader. The leader can remind the group of the main topics and then proceed around the table for issues/problems. The key to a successful huddle is for each issue identified to be assigned an owner responsible for follow-up. Huddles should provide an opportunity to “look back” to solve any issues from the previous day and “look forward” to help prevent any failures. The roundtable reporting should be done by exemption only with each participant in the roundtable responding with a report or either with “no concerns” or “nothing to report”.
Just as with any other plan, you can establish metrics around your huddles to determine if the process is helping you with the overall improvement plan. (For example, your team might decide that huddles would be a helpful process in reaching the outcome goal of 100% flu vaccination on 100% eligible patients. To help measure the effect of this intervention your team sets process goals around the huddle.)
1. “We will have daily huddles before 10am 90% of the time by January 15th”
2. “All clinical departments will be represented at the huddle.”
3. “The huddle will last no more than 15 minutes.”
Staff Incentive Program
Many facilities have decided to link quality performance to the staff member’s individual job evaluation. Examples of linking quality performance with employee performance are:
• incentives for staff when performance is met; or
• evaluating the employee on the number of successful screens or evaluations.
Understanding Errors and Near Misses
It is essential that errors or near misses are included in data collection and reviews. Errors are typically those incidences that reach the patient and near misses are events that are caught and corrected prior to reaching the patient. Your facility may decide to track errors and near misses through your event or incident reporting system and a Root Cause Analysis may be performed. Near misses should be carefully reviewed since these types of mistakes can often provide great insight into problem-prone errors and when reviewed, can help to prevent an actual error from occurring.
Root Cause Analysis (RCA)
A root cause analysis (RCA) is simply a process to help caregivers, quality leaders and physicians determine how an error occurred. We often think most about doing an RCA when a major or serious safety event occurs but, an RCA can be done for any error. It may be especially important to perform an RCA on an error or near miss that has occurred more than once to prevent recurrence.
If you have been performing RCAs at your facility, you may be performing these by gathering a group of individuals around the table to discuss what happened. Interviews conducted by a quality leader prior to the team coming together to discuss and develop an action plan can be a more time efficient method of performing an RCA.
Failure Modes Effect Analysis (FMEA)
A Failure Modes Effects Analysis (FMEA) is an excellent tool for evaluating potential problems when a new or revised process is being implemented. A FMEA process determines occurrences and helps a team assign levels of risk or impact to the success or desired outcome of process. The Institute of Healthcare Improvement (IHI), has numerous resources in its QI Essentials toolkit. This toolkit is available for free at www.ihi.org by creating a log-in identification.
Fishbone Diagram
The Fishbone Diagram, (Appendix C), demonstrates a clear explanation of the advantages of considering people, processes or equipment impacting the team’s ability to meet defined goals.